Reimagining Youth Behavioral Health Needs with Empowerment Counseling Services
.png)
Introduction
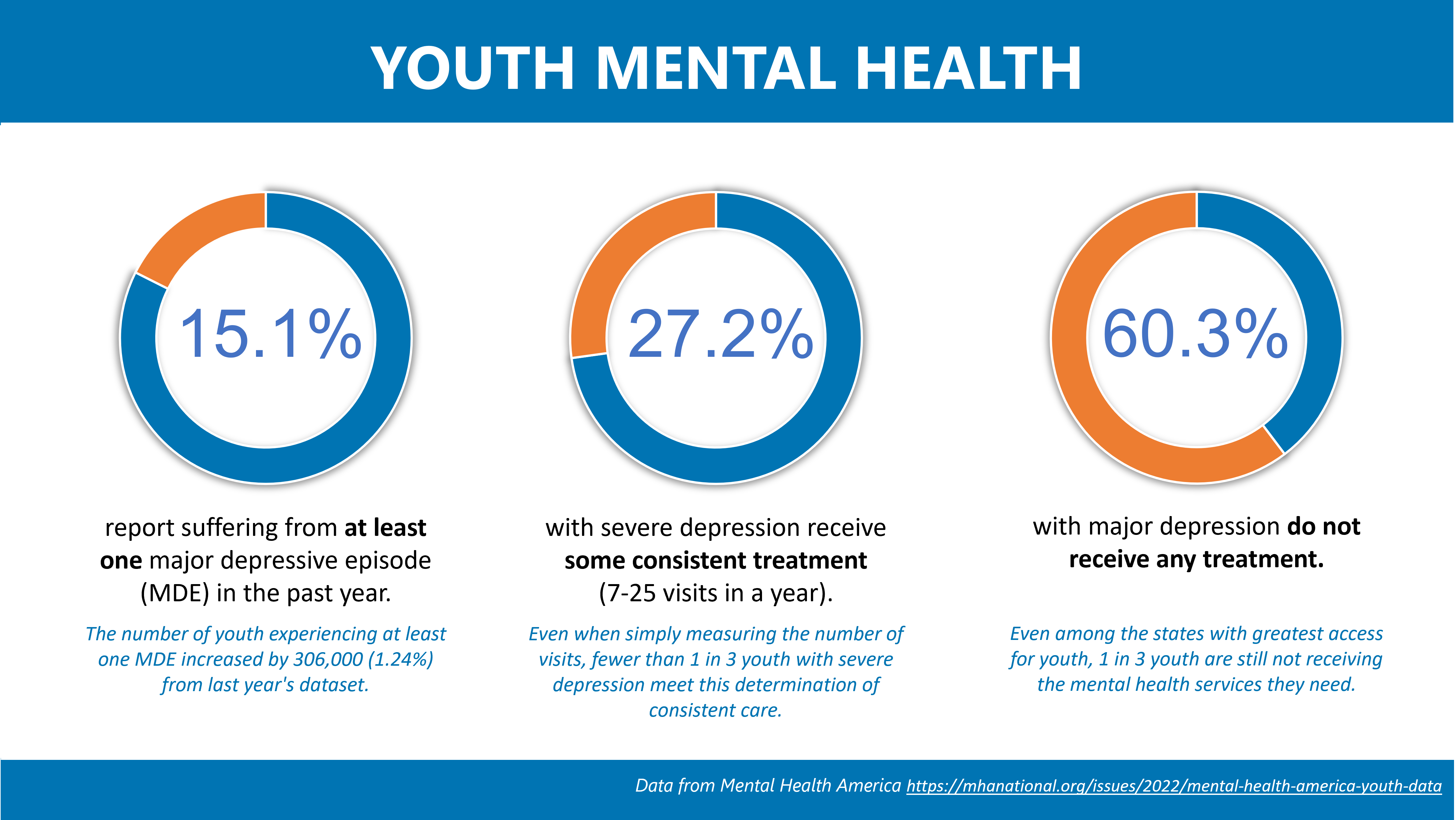
Already in dire circumstances, mental health in the United States has continued to worsen throughout the COVID-19 pandemic. Statistics for child and adolescent mental health are concerning, with significant increases in the number of youth experiencing moderate to severe anxiety and depression. Even as schools have returned to in-person learning and social isolation has decreased, the national well-being of children and youth remains precarious. From February 21 to March 20, 2021, mean weekly emergency room visits for suspected suicide attempts were 51% higher for adolescent girls and 4% higher for adolescent boys compared to early 2019.
Increasing Need, Increasing Barriers
For children and families navigating mental health challenges, access to care and the cost of receiving care can be prohibitive factors. However, when children experience severe behavioral health needs and require more intensive treatment, the barriers only increase. These severe behavioral health conditions can have a detrimental effect on quality of life both for the child and their families. According to a report released by the Medicaid and CHIP Payment and Access Commission (MACPAC), children with significant mental health conditions are less likely to finish high school and attain higher education. They are also at an increased risk for institutional placements, co-occurring substance use disorder, and suicidal thoughts and behaviors.
Emergency department visits, inpatient admission, or other residential treatment facilities are not only disruptive in that they remove the child from their home, school, and community, but are also costly and can have months-long wait lists to even begin treatment. Services provided within the home setting or in the community can help minimize disruption, decrease costs, and improve outcomes for success.
Intensive In-home Services
As health care costs increase and the number of children with mental health needs increase, identifying alternative methods for treatment that reduce costs while still providing quality, effective care is critical. One approach demonstrated to be clinically effective is intensive in-home family intervention (IIFI).
IIFI is a team-based therapy service provided face to face to the youth in their living arrangement and within their family system. The model addresses symptoms and behaviors that, as the result of a mental health or substance use disorder, put the child and/or others at substantial risk of harm. IIFI is a service intended to improve the functioning of the youth and their family by clinically stabilizing the living arrangement and preventing the utilization of higher-end services such as crisis stabilization or acute inpatient psychiatric residential treatment. This comprehensive approach includes individual and family therapy, cognitive behavioral therapy, skills coaching and case management services. Clinicians working with the youth and their families in the home allow for optimization and implementation of a patient-centric therapy plan. The program typically is 6 months and includes a team available to the family 24/7 for crisis intervention, phone coaching and other resources. At the end of the program, the youth will then transition to community-based services and to outpatient therapy to continue intervention. Studies on IIFI have demonstrated that this outpatient treatment method can be effective and avoids the need for higher level and more expensive interventions that require children to be separated from their families.
Regence Health Policy Center spoke with Andree Miceli, LCSW, Behavioral Health Clinical Director at Regence Blue Cross Blue Shield, and Amanda Escobedo, Director of Operations at Empowerment Counseling Services, to learn more about IIFI treatment and the potential it has to lower costs and improve outcomes for youth and their families. Empowerment Counseling Services is a community-based, mental health agency based in Utah, providing services to Davis, Salt Lake, and Weber counties.
One of the interventions Empowerment Counseling Services provides is intensive in-home family intervention. Why are these services unique? How does this model compare to other intervention models in terms of patient and family outcomes and satisfaction?
“Our Intensive In-Home Services provide services in the very environments in which the difficulties are happening, typically home, school, peer group and employment. Services are tailored with individualized treatment plans for each family’s unique area of need. The goal of our model for intensive in-home services is to customize treatment to the root of the problems. In our experience in providing in-home services for over 20 years, we have found there are multiple layers of issues that are behind the behaviors that the child may be experiencing. The evolution of our agency’s model connects back to the family preservation model and includes a shift toward holistic treatment of families in their homes.
Our Intensive In-Home Services take place in the very environments in which the difficulties are happening: home, school, peer group and employment...Our model strongly focuses on empowerment and teaching the family how to manage and prevent their symptoms while being able to practice these strategies in the environment in which they are occurring.
Our model takes a holistic approach and looks at the whole environment of the child including any genetic vulnerabilities to mental health issues or predisposition, parenting, home environment, school, social and financial support, all stressors that could be triggering or exasperating manageable symptoms in family issues. Our model strongly focuses on empowerment and teaching the family how to manage and prevent their symptoms while being able to practice these strategies in the environment in which they are occurring.” -Amanda Escobedo, Empowerment Counseling Services
What are the benefits of in-home services as compared to traditional models of outpatient therapy or inpatient treatments in terms of outcomes, quality of care and costs?
“Because we are able to see the entire family system and the direct reflection of the issues manifested in the home environment treatment can be addressed at multiple levels immediately, and family momentum and sense of team can be engaged whereas in out-patient therapy it can take months to be able to clearly recognize the root of the problem.
When we are able to work more long-term with a family, we have noticed significant changes in all family members and preventative progress in preventing secondary problems in siblings or family members impacted by the primary client issues.
Our services are intended to be very flexible to the family while they are in crisis then taper down while being available to return back into the home during regressions or unpredicted stressors. The Model emphasizes a solution-focused, family system and multi-systemic therapeutic clinical model. Our experience has been that to treat the client and family in the home environment has a long term impact on a child sustaining progress and moving away from treatment dependency, out of home placement, or higher levels of care. When we are able to customize treatment to be intensive during times of crisis and taper out in times of stability, there is a very positive continuum of care that has consistency and predictability verses starting with a new worker and new treatment every time that a crisis or issue occurs.
Our experience has been that to treat the client and family in the home environment has a long term impact on a child sustaining progress and moving away from treatment dependency, out of home placement, or higher levels of care.
We consistently receive referrals for cases that have had hundreds of thousands dollars of treatment including residential, day-treatment, and hospitalization because [these modalities] do not treat the root problem in the home including the parents or being able to coordinate a family’s needs for long-term resources.” -Amanda Escobedo, Empowerment Counseling Services
COVID-19 increased the use of telehealth and other remote care options. From the payor perspective, how do you see these innovations impacting access to behavioral care? What technological advancements have you seen that have the potential to further improve access to behavioral health services?
“As of January 2020, Regence had about 1.5% of behavioral health visits provided through telehealth. In April of 2020, this number rose to 63.2%. In 2022, we still see approximately 53% of visits performed through telehealth. Along with this, many facility-based programs offered Intensive Outpatient services virtually and continue to do so. Telehealth improves access as it allows members who live a great distance from programs to be able to attend where otherwise the distance and travel would be a barrier. Providers can reach a much wider radius of Regence members. Many office-based providers also added telehealth visits for members and continue to do both [in-person and telehealth]. We have also seen a growth in digital options for behavioral health services including self-help and wellness programs. The digital space continues to grow.” -Andree Miceli, Regence
What barriers exist to growing and scaling this type of home-based care model? Are there policies or legislative actions that could advance adoption of home-based care models?
“Barriers we see are new provider acquisition and the length of time it takes for new providers to obtain credentials. Additionally, master’s level supervised clinicians are unable to provide services with many commercial plans until they are fully licensed.” Amanda Escobedo, Empowerment Counseling Services
“One main requirement is that the in-home team is led by a licensed clinician for credentialing and billing purposes. Policies which require clinical-led teams would help. Another barrier is the codes a particular program uses to bill and their compatibility with codes Regence can pay due to claims system limitations. Typically, these programs [intensive in -home services] focus on Medicaid so they are billed use Medicaid codes, which are not always compatible with commercial insurance payment systems. If these were more in sync the process would be easier. Another barrier from the payor side is contracting with virtual providers. Even though a provider is licensed to provide behavioral health services in their own state(s), because they are virtual and may not physically reside in our 4-state market (Idaho, Oregon, Utah, Washington), it requires a different type of contracting which can take longer and can be more complex.” -Andree Miceli, Regence

